Overview
The Epilepsy Society MRI Unit, Chalfont St Peter, Buckinghamshire and is located in a dedicated building adjacent to the newly opened Epilepsy Society Research Centre.
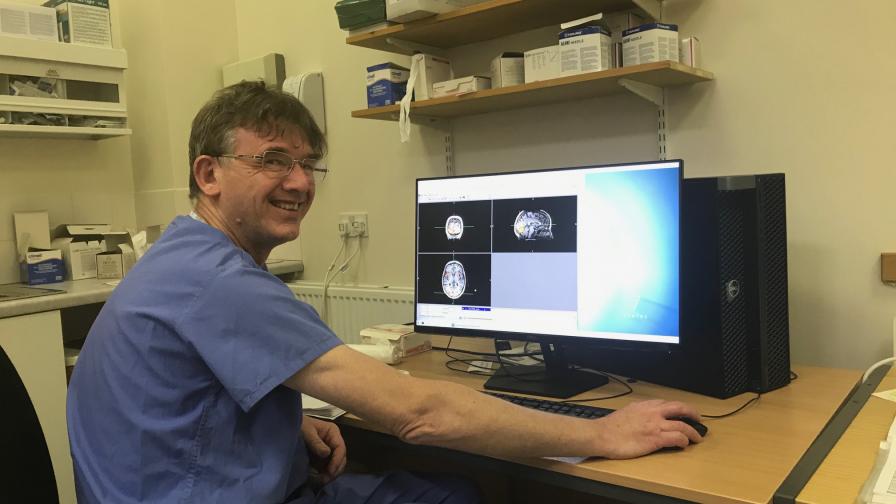
In 2019, there was a major upgrade to the Chalfont MR scanner to enable increase resolution, particularly of diffusion and functional MRI that show the nerve fibre connections in the brain and the parts of the brain that are critical for language and memory.

Epilepsy Society's MRI Unit is key component of extensive collaborations with UCL, The greatly enhanced connectivity and the state of the art scan storage facility enables scan data to be accessible, with colleagues at other locations.
The acquisition of MRI data at The Chalfont Centre is crucial, as it is co-located with the Gowers Centre and outpatients and research MRI can be acquired at the same time as clinical MRI. Valuable image analysis is also carried out on MRI scans that are obtained for clinical purposes, which is a fundamental tenet of the UCLH-UCL shared vision of having a Research Hospital.
Our research areas
Our new retrospective study aims to investigate the impact of medical and surgical epilepsy treatments on cognition, such as language and memory. We intend to use existing clinical information from patients under our care for this research project, which has been approved by UCL, UCLH, and the Health Research Authority (HRA). No individual will be identifiable from the results of this analysis.
If any person wishes for their information not to be used in this study, they can contact the study coordinator and chief investigator, Professor John Duncan by email (j.duncan@ucl.ac.uk), telephone (020 3448 8612), or by post on the below address.
Any decision not to have your information included in this research study will in no way affect your future medical care.
Prof John S Duncan, MA, DM, FRCP, FMedSci
Box 29, National Hospital for Neurology and Neurosurgery
Queen Square, London, WC1N 3BG
Optimising epilepsy surgery
Discover how the removal of the temporal part of the piriform cortex greatly increases the chances of seizure freedom after temporal lobe resection for temporal lobe epilepsy.
Analysis of brain structure
Identifying focal abnormalities that underlie refractory epilepsy is crucial in the consideration of epilepsy surgery.
Machine learning and quantitative MRI
We have created a multivariable AI based program to identify covert abnormalities in individuals who are considering surgery and validating this with the sites of seizure onset in individuals having intracranial EEG at NHNN.
Functional MRI (fMRI)
In the last 20 years we have been using functional MRI (fMRI) at Epilepsy Society's Chalfont Centre to map where different functions such as language and vision occur in the brain.
Language
fMRI can show where in the brain language and memory is carried out. This enables us to predict the risks of surgery and lateralise language functions pre-surgically our next step is to use this information to design surgery that does not affect language.
Memory and brain function
Difficulties with language and memory are a significant issue in people with epilepsy. Epilepsy surgery may be a suitable treatment option in some people however in some there is worsening of language and memory functions that can significantly impact of quality of life.
Understanding the effects of medication and Pharmaco-fMRI
Adverse effects of epilepsy medication has a very negative effect on quality of life. Functional MRI (fMRI) can show the brain activation that underpin language and memory and thought.
Inflammation and blood brain imaging
Depression, is common in epilepsy. Brain inflammation occurs in epilepsy and depression. We will use novel MRI to demonstrate this brain inflammation that may give rise to seizures and depression so that we may identify effective therapies.
The Chalfont Centre MRI Team
Meet the The Chalfont Centre MRI Team at Epilepsy Society, leading the way in neuroimaging.
Neuroimaging research areas and projects
Read about current research areas and projects running under our world leading neuroimaging programme.
Neuroimaging Innovation
Find out about our innovative Epilepsy Navigator software that enables even more sophisticated and accurate brain surgery for epilepsy.
Research papers
We've compiled a summary of our latest research papers for you to read, written by our powerhouse multidisciplinary team who contribute to a wide ranging spectrum of epilepsy research.
This includes PhD theses from the ES MRI Epilepsy Imaging Group.
These papers give you a snapshot of our teams clinical and research knowledge, which is helping us to further our understanding of people with epilepsy.
Teaching
Every March for the last 3 years Professor Matthias Koepp has organized the International League against Epilepsy Neuroimaging course, at Chalfont MRI and Research Centre. This is very highly regarded internationally, with delegates coming from all over the world, and is always oversubscribed.
Future look
In 2021 we will continue our current research priorities of imaging language and memory and the structural basis of these in epilepsy, and to visualize multimodal data in 3-dimensions for the optimization of epilepsy surgery. We will further link imaging data with genetics in the ENIGMA project.
We will set-up imaging of inflammation and break-down of the blood-brain-barrier in epilepsy, and will explore the effects of anti-epileptic drugs on the brain.
We will explore the possibility of using MRI as an adjunct to post-mortem examination of individuals who succumb to SUDEP, to try to better understand the causation of this tragedy.
In the next 5 years, epilepsy imaging research will need access to a 7T MRI scanner, if we are to be globally competitive and to have this linked with a MEG facility using novel mobile MEG technology and PET.

Reading brain scans through Artificial Intelligence
Researcher Baris Kanber explains how machine learning - or Artificial Intelligence - could enable more people with uncontrolled seizures to achieve seizure freedom.
Funding
Epilepsy Society supports the MRI scanner and the premises and pays the salaries of radiographers, administration and part of Prof MJ Koepp’s and Dr M Sidhu’s salaries. Other salaries are supported by Epilepsy Society (Sobell Foundation), UCL, NHS, NIHR senior investigator award and NIHR Biomedical Research Centre, Wellcome Trust, MRC, Epilepsy Research UK, Newton Foundation.
Contact us
Epilepsy Society MRI Unit, Chesham Lane, Chalfont St Peter, SL9 0RJ
Tel: +44 (0)1494 601360 - Fax: +44 (0)1494 875945
Neuropathology
The Epilepsy Society Brain and Tissue Bank is the first of its kind in the UK. It is dedicated to the study of epilepsy through brain and other tissue samples.
Research
The ultimate goals of our current research are to spearhead personalised treatment and to incorporate genomic diagnosis into the NHS for people with epilepsy.
Genomics
Read how we are working to understand the genetic architecture of each individual person's epilepsy through our world leading genomics research programme.